blocking the beta adrenergic receptors on heart
and blood vessel cells. Propranolol and aging have
For years, scientists were puzzled by this phenom-
the same effects, according to a number of studies.
enon, but they may be getting closer to under-
Older hearts and blood vessels, apparently, have
standing how and why these messages get muffled.
blocked some of these beta adrenergic receptors.
In particular, investigators are looking at the sympathetic nervous system, the part of the autonomic
Investigators soon found that with age the number
nervous system that signals the heart to speed up.
of beta adrenergic receptors on heart cells did
This subsystem helps regulate the heart beat
diminish. But this reduction was only modest.
through a series of signals passed from neurotrans-
Instead, studies now suggest that something else
mitters to receptors on the membranes of heart
about these receptors changes with age: the
cells. One of these important signaling cascades
number of them that are capable of binding with
starts when neurotransmitters, such as cate-
catecholamines, i.e., those in a “high affinity state,”
cholamines, bind to special protein molecules,
seems to decline with age.
called beta adrenergic receptors, on the heart cell
The reason for the reduced response could lie any-
membrane. Once activated by a neurotransmitter,
where in the cascade of events in heart muscle
these beta adrenergic receptors set off a chain of
cells that occurs after catecholamine binds to the
molecular events that allows more calcium to enter
receptor. Scientists are finding a host of possible
heart cells. Increased calcium within these cells
cellular mechanisms that might explain the
can lead to a stronger and more rapid heart beat.
reduced response. They hope once these mecha-
But as we get older, something goes awry in this
nisms are better understood, they will be able to
signaling cascade. As a result, the older heart
find a way to mend the link or prevent it from dis-
can’t respond to these neurotransmitters, so it
rupting messages in the first place. Eventually
doesn’t react to stress as well as a younger heart.
such findings could lead to new ways to prevent
During exercise, for instance, an older heart is less heart failure. •
19

C E L L U L A R Clues
The sustained dependability of a tireless heart relies…on the performance of the trillions of chemical reactions occurring in its aggregate of cells every instant of its function.
SHERWIN NULAND, MD, AUTHOR OF THE WISDOM OF THE BODY, 1997
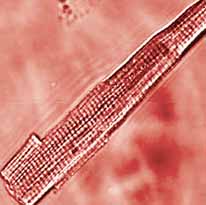
Under a microscope, the true grandeur of the heart
that changes an electrical impulse into a muscle
reveals itself. Magnified, a rod-shaped heart muscle
contraction. These discoveries have led to novel
cell taps out a constant beat. A closer look within the hypotheses about aging and disease. Scientists have
cell reveals a series of thin contractile fibers called found that age-related changes in heart muscle
myofilaments that are the machinery driving these
cells (myocytes) help explain alterations in the
contractions. In the left ventricle alone, there are
heart as a whole. For instance, they’ve learned there nearly 5 billion of these cells beating rhythmically, as are fewer myocytes to
if they are all listening to the same snappy tune.
do the work as we age
and those that remain
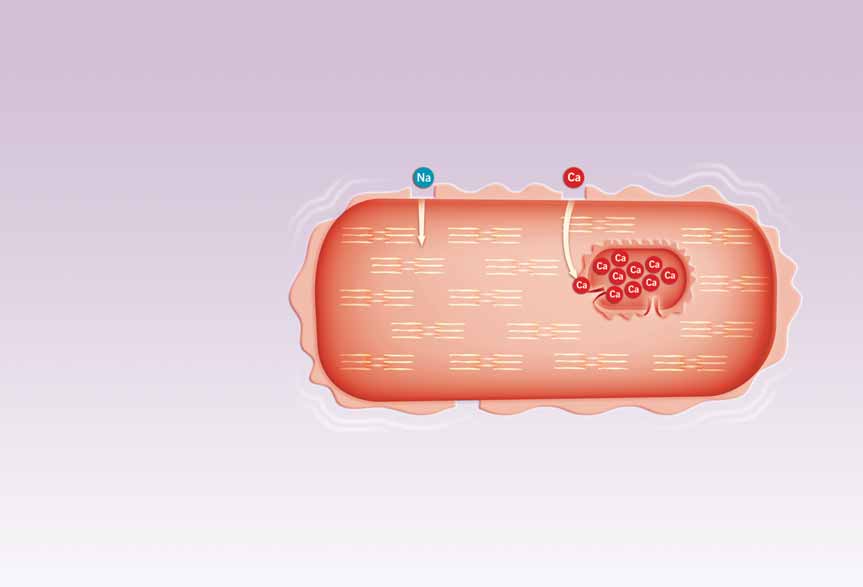
The chemical chain of events that underlies the
enlarge, compromising
beating of these cells and of the heart as a whole is their ability to pump
truly remarkable. First, there’s the electrical
blood efficiently. They’ve
impulse along the cell’s membrane; then channels
also discovered much
open in the cell membrane allowing sodium to
about how these changes
flow into the cell. After that, more channels open
could interact with dis-
and calcium enters and binds to a tiny structure
ease processes and found
near the membrane; then, much more calcium
clues to how exercise
explodes out of that structure into the cell’s inner
affects the biochemistry
fluid and combines with a myofilament protein
Magnified, a rod-shaped heart
of cells. Scientists have
called troponin. Troponin then changes shape to
muscle cell (myocyte) contracts its
begun to question some
allow two other proteins, actin and myosin, to come
myofilaments. Billions of these
of the long-held theories
together. The joined proteins slide past each other
cells contracting in synchroniza-
about the nature of the
tion produce a heart beat.
in such a way as to shorten the cell, pulling the ends aging heart, including
of the cell inward—this is the actual contraction—
whether some myocytes can replicate and what
and then the whole process reverses itself as the
role aging may have in this process. And they’ve
heart relaxes in preparation for the next beat.
learned a great deal more about the critical role
During the past 30 years, scientists have made
calcium plays in the drama of the aging heart.
some intriguing discoveries about the process
21
The Marvelous Calcium Pump
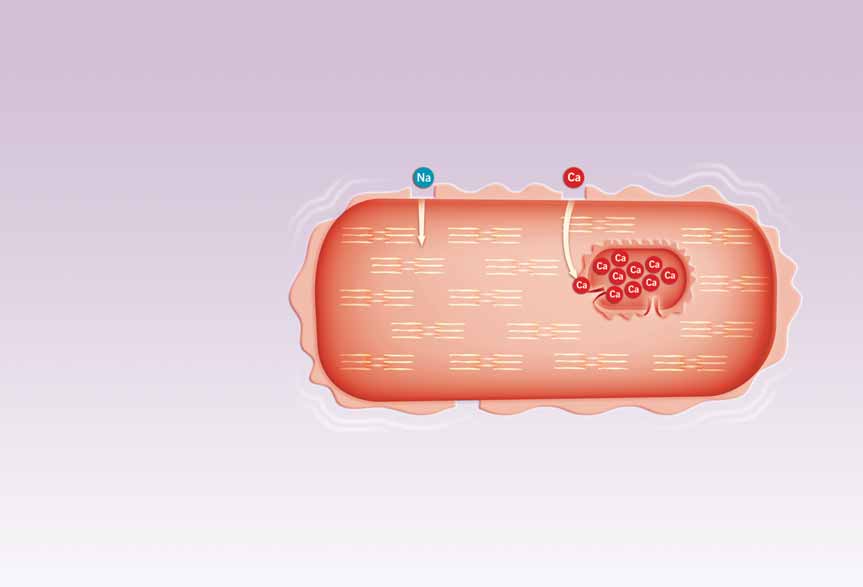
This tiny bit of calcium binds to openings called
calcium release channels on the sarcoplasmic
Scientists have long known that calcium—the
reticulum, an organelle (a small cellular “organ”)
mineral that helps keep your teeth and bones
that serves as a storage bin for calcium. In
strong—also has an important job within your
response, the sarcoplasmic reticulum releases a
heart. Calcium entering the myocyte’s inner fluid
large amount of its stored calcium into the cell.
or cytosol binds with other contractile proteins to
The calcium released from this storage compart-
bring about contraction. Calcium leaving the
ment binds to the cell’s myofilaments, causing
cytosol allows the cell to relax. It’s this constantly them to tighten or shorten. As the myofilaments
changing ebb and flow of calcium in and out of the
tighten, the myocyte compresses (shrinking in
cytosol of heart muscle cells that is the essence of the length and fattening in width). This process
heart beat. (See How a Myocyte Contracts, page 23) occurs almost simultaneously in every cell in the
heart wall, causing them to contract and pump
blood out of the heart.
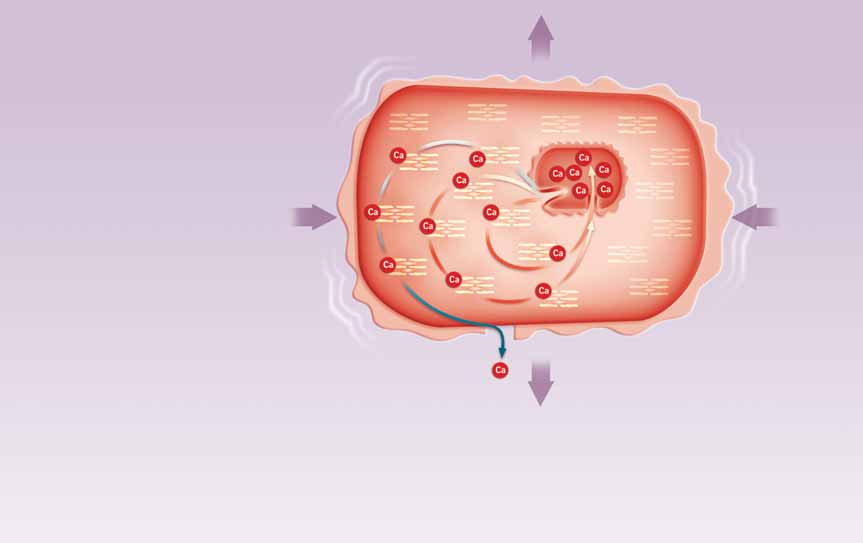
In order for the heart to relax, the cycle winds
down and calcium detaches from the myofilaments.
A cellular mechanism kicks in and pumps most of
the calcium back into the storage bins located in
the sarcoplasmic reticulum. Any residual calcium
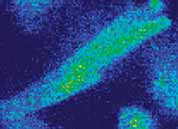
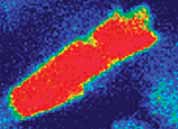
Between heart beats, calcium levels (red) diminish in a myocyte’s is driven out of the cell through specialized exit
inner fluid or cytosol, allowing it to relax (left). During con-calcium carriers located on the cell’s membrane.
traction, a large amount of calcium surges out of a myocyte’s These carriers are proteins that swap calcium
sarcoplasmic reticulum, right, triggering tightening or short-inside the cell for sodium outside of it. Then the
ening of the cell’s muscle fibers (right). This process occurs cycle restarts in preparation for the next heart beat.
almost simultaneously in every cell in the heart wall, causing them to contract and pump blood out of the heart.
If this system fails, and calcium cycling gets out of whack, chaos can ensue. The heart, for instance,
At the beginning of the calcium cycle—which
can’t relax and fill with blood properly and diastolic coincides with the heart filling with blood—
pressure in the heart increases. In addition, indi-
calcium in the cytosol and surrounding the con-
vidual cells may fire off rapidly and independently,
tractile filaments of each myocyte is at least 10,000
resulting in arrhythmias—variations from the
times lower than calcium levels in your blood and
normal heart beat rhythm—and fibrillation,
in other fluids between your cells, called the intercel-which is a very rapid twitching of individual
lular spaces. As the cycle progresses, pores (or
muscle fibers. In particular, older hearts are more
channels) in cell membranes open and close,
susceptible to spontaneous calcium oscillations
allowing various salts to flow in and out of the cell.
than younger hearts, and it takes fewer oscillations
This activity triggers momentary fluctuations in
to bring about fibrillation. Fibrillation in the left the positive and negative electrical charges across
ventricle leads quickly to acute heart failure and to the cell’s membrane. When these fluctuations
death if not treated.
reach a particular threshold, an electrical discharge Heart failure occurs when the heart loses its ability occurs. This discharge, called the action potential,
to pump enough blood to meet the body’s
essentially flips a switch on the myocyte’s mem-
requirements. In particular, heart failure causes
brane to open pores that allow a small amount of
the heart to gradually lose its reserve pumping
calcium to enter the cell.
22
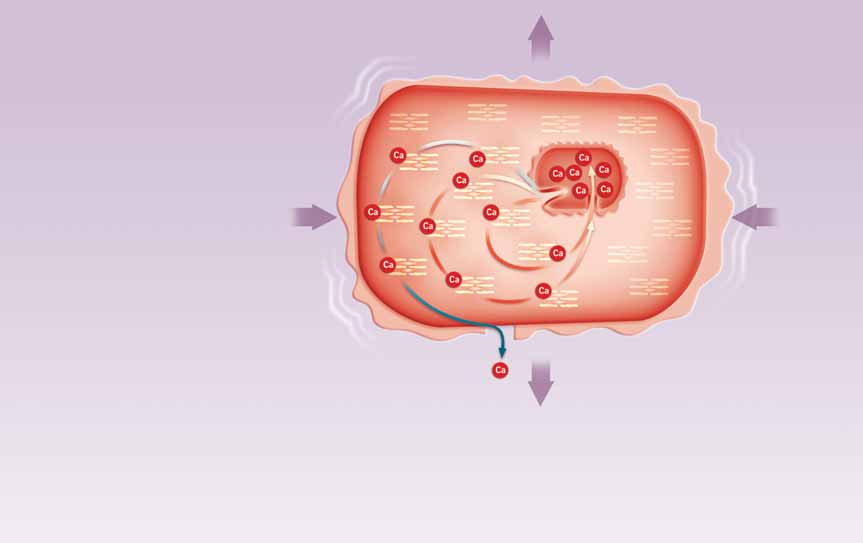


How a Myocyte Contracts
Sarcoplasmic
Reticulum
Relaxed
1
2
Action Potential
Sodium ( Na ) channels
1
open in membrane
causing change in
electrical charge.
3
This causes surface
2
membrane Calcium
( Ca ) channels to open,
causing small Ca influx.
Calcium binds
3
to calcium releasing
channel protein on
Contractile Protein
sarcoplasmic reticulum.
(before contraction)
Calcium
Pump Protein
Calcium Releasing
Channel Protein
Contracted
A large amount of
4
calcium is released from
sarcoplasmic reticulum.
4
Ca
Calcium activates the
5
contractile proteins.
Cell contracts.
6
Calcium disengages
5
6
from the contractile
proteins. Most is
CONTRACTS IN LENGTH
pumped back into the
sarcoplasmic reticulum.
Some calcium leaves
7
the cell.
Contractile Protein
FATTENS IN WIDTH
Cell relaxes and cycle
(during contraction)
7
renews.
23
capacity and work less efficiently. Blood pressure
reticulum and then awaits the next signal to do its
and flow to body organs drops. The kidneys sense
job again. Scientists began taking a closer look at
this and send out signals prompting retention of
this mechanism when they learned that muscle
body fluid, which contributes to swelling. This can
from older hearts takes longer to relax than muscle
cause a backup of fluid into the lungs and body
from younger hearts. One of the prime suspects
tissues triggering shortness of breath, swelling of
for this phenomenon was calcium. To test this
the legs and feet, and other symptoms. As heart
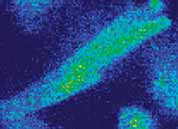
idea, Dr. Lakatta and his colleagues at the NIA used
failure progresses the effects can become quite
a protein that binds to calcium and gives off a blue
severe, and patients often lose the ability to per-
light to detect how much calcium is in a cell at any
form even modest physical activity. Eventually, the
one time. When they injected this calcium-sensing
heart's reduced pumping capacity may interfere
protein into myocytes within heart muscle in lab-
with routine tasks, and individuals may become
oratory dishes, the blue light showed that calcium
unable to care for themselves. Heart failure rises
levels, after a contraction, fell more slowly in older exponentially with advancing age, and studies of
myocytes. Or, putting it in biologists’ terms, the
the calcium cycle in heart cells suggest a number
cytosolic calcium transit was longer. But why?
of possible reasons.
Could the calcium be spending longer in the inner
fluid because the sarcoplasmic reticulum wasn’t
When a Good Pump Goes Bad
removing it as quickly in older cells?
Imagine sitting calmly in a living room chair when
The answer was yes. In experiments, NIA scientists
the smoke detector goes off. As you scramble to
isolated the sarcoplasmic reticulum from the rest
quickly get out of the house, your heart starts
of the heart cell, placed it in a test tube, and then beating faster. A few moments later, after you
added calcium. The sarcoplasmic reticulum took
discover it was a false alarm, you return to your
up the calcium more slowly in samples from older
comfortable chair, and your heart rate slows
animals than those from younger ones.
again. As this scenario suggests, your heart beat
Subsequent studies confirmed that the sarcoplasmic
can vary from moment to moment. And your
reticulum—or more precisely, a protein on this
heart’s ability to respond to these changes depends
organelle—removes calcium more slowly in older
a lot on calcium. The more calcium your heart
hearts. Researchers have found that older cells
cells release from their intracellular storage bins,
have lower amounts of this particular protein,
the greater the force of the heart’s contractions.
often called the calcium pump protein because it
But how well these mechanisms work depends on
removes the calcium in a series of repeated move-
how much calcium can be pumped from these
ments. In essence, the sarcoplasmic reticulum
storage bins between heart beats. In young hearts,
removes calcium from the inner fluid more slowly
these calcium pumps work quite well, but in older
in older hearts because there are fewer pumps,
hearts these pumps are much less efficient.
and those that remain don’t work as well because
After the heart beat, if you recall, most of the calcium of communication breakdowns between the brain
returns to the storage bins in the sarcoplasmic
and the heart.
Like other changes, the longer calcium transient appears to be one way that the heart adjusts to age, or more specifically to the stiffer arteries that accompany aging.
Unfortunately, like those other changes, this adjustment also has a cost.
24
If these pumps aren’t working properly or have
Age Lengthens Action Potential
shut down, the sarcoplasmic reticulum won’t fill
In addition to calcium transit, two other clusters
as well as it should with calcium, and there won’t
of events in myocytes seem to be affected by age.
be enough calcium to fulfill the heart cells’ needs,
particularly during exercise or stress.
One is the action potential. This is a transient
alteration in the amounts of positive and negative
Once scientists learned about the pump protein,
charges on either side of the myocyte membrane.
the next question was about that protein’s gene.
As mentioned earlier, the action potential triggers
Proteins make up a huge category that includes
the opening of sodium and then calcium channels
enzymes, growth factors, hormones—almost all
in the membrane.
the substances that are responsible for the day-to-
day functioning of living organisms. Proteins are
The action potential is prolonged in older hearts
produced by genes in the nucleus of every cell.
and may contribute to the longer calcium tran-
Each protein has its own gene. Cells translate gene
sient. This occurs because as the heart ages, there
codes into proteins through a complex, multistep
are coordinated declines in both the activity
process called gene expression. Any alteration in
and number of proteins involved in the action
this process can lead to changes in the end product,
potential as well as the proteins that respond to its the protein.
signals. A longer action potential generates a
longer calcium transit, which in turn, produces
In the case of the pump protein, the gene that
a longer contraction. Each of these processes is
produces it is only about half as active in older
controlled by specific proteins.
hearts as in younger hearts. The end result of all of these changes is a decline with age in the maxi-The prolonged action potential helps older hearts
mum strength of the heart beat during strenuous
work well in most situations. It does this in two
activity. Reduced calcium pumping also prolongs
ways. First, pores on the myocyte’s membrane
the time it takes for heart cells—and in turn, the
stay open longer to allow more calcium to enter
heart as a whole—to return to a relaxed state. As a
the cell between beats. Second, the proteins that
consequence, the heart can’t fill with blood as
carry calcium out of the cell and sodium back
readily as it once did and prepare for the next
in work more slowly. The net result is that more
heart beat.
calcium is available within the cell. These effects
allow the weaker sarcoplasmic reticulum—which
Like other changes, the longer calcium transient
has fewer pumps—to load up on calcium in prepa-
appears to be one way that the heart adjusts to age,
ration for the next beat. But these adjustments,
or more specifically to the stiffer arteries that
like so many other cardiovascular adaptations,
accompany aging. Unfortunately, like those other
may have a downside. For instance, in an aging
changes, this adjustment also has a cost.
heart the long action potential adaptation works
“It makes sense from an engineering standpoint
well at slower heart rates. But during a rapid heart
to have a longer contraction if you’re pumping
rate, the longer action potential contributes to
blood into stiffer vessels,” Dr. Lakatta says. “The
calcium dysregulation of myocytes. As a result,
downside is that when you alter the dynamics of
the older heart doesn’t respond as dynamically
calcium, various stresses can more easily throw
to the needs of the body as a young heart. So, a
the calcium out of balance. One consequence of
prolonged action potential is yet another possible
this is that an older person is more apt to feel short reason that an older person usually can’t do as
of breath during vigorous exercise.”
much exercise as someone younger.
25
Prolonged contractions also allow the older heart to eject blood into the arteries later in the heartbeat. This adaptation is good because it improves the blood flow through an older person’s stiffer arteries.
Contractile Proteins
actually help the older heart work more efficiently.
That’s because slower and longer contractions
The other mechanisms that change with age
don’t use as much energy. Prolonged contractions
involve contractile proteins—actin, myosin, tro-
also allow the older heart to eject blood into the
ponin, and others—that interact to shorten, or
arteries later in the heartbeat. This adaptation is
contract, the myocyte. These contractile proteins
good because it improves the blood flow through
pass through a series of steps, triggered by
an older person’s stiffer arteries.
calcium, which bring actin and myosin together
into crossbridges. The crossbridges use energy
Free Radical Damage
released during the transaction to shorten the cell.
With age, one part of the crossbridge alters—the
Myocytes produce free radicals, unstable oxygen
part called the myosin heavy chain.
molecules that can disrupt a cell’s inner workings.
As the heart ages, these free radicals can greatly
The myosin heavy chain can be produced in two
alter how well the cellular calcium pumps on the
slightly different forms, one dubbed alpha, the
sarcoplasmic reticulum work.
other beta. In experimental animals, the alpha
myosin heavy chain decreases with age, while the
In myocytes, most free radicals are produced in tiny
beta increases. The same seems to be true in the
cellular organelles called mitochondria and by an
human atrium. When the proportion of alpha
enzyme in cell membranes called NADPH oxidase.
myosin heavy chain is reduced in isolated cells, the
Mitochondria convert oxygen and food into an
contraction speed is slower.
energy-releasing molecule that powers most cellular
processes. But during this process they also produce
Changes in the myosin heavy chain have been
potentially harmful byproducts such as oxygen free
traced back to the genes involved—alpha is
radicals. A free radical can be produced by almost
expressed less with age, beta more. The expression
any molecule when it loses an electron from one or