Are you at risk of type diabetes I-II?
Diabetes Type I-II
What is diabetes?
Diabetes is the condition in which the body does not properly process food for use as energy. Most of the food we eat is turned into glucose, or sugar, for our bodies to use for energy.
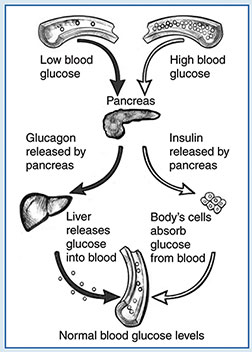
The pancreas, an organ that lies near the stomach, makes a hormone called insulin to help glucose get into the cells of our bodies. When you have diabetes, your body either doesn't make enough insulin or can't use its own insulin as well as it should. This causes sugars to build up in your blood.
This is why many people refer to diabetes as “sugar” Diabetes can cause serious health complications including, heart disease, blindness, kidney failure, and lower-extremity amputations.
Diabetes is the seventh leading cause of death in the United States.
How prevalent is diabetes among blacks?
-
Blacks are 1.7 times as likely to develop diabetes as whites.
-
The prevalence of diabetes among blacks has quadrupled during the past 30 years.
-
Among blacks age 20 and older, about 2.3 million have diabetes – 10.8 percent of that age group.
-
Blacks with diabetes are more likely than non-Hispanic whites to develop diabetes and to experience greater disability from diabetes-related complications such as amputations, adult blindness, kidney failure, and increased risk of heart disease and stroke.
-
Death rates for blacks with diabetes are 27 percent higher than for whites.
What are the symptoms of diabetes?
People who think they might have diabetes must visit a physician for diagnosis. They might have SOME or NONE of the following symptoms:
-
Frequent urination.
-
Excessive thirst.
-
Unexplained weight loss.
-
Extreme hunger 1.
-
Sudden vision changes.
-
Tingling or numbness in hands or feet.
-
Feeling very tired much of the time.
-
Very dry skin.
-
Sores that are slow to heal.
-
More infections than usual.
Nausea, vomiting, or stomach pains may accompany some of these symptoms in the abrupt onset of insulin-dependent diabetes, now called Type 1 diabetes.
What are the types of diabetes?
Type 1:
Type 1 diabetes, previously called insulin-dependent diabetes mellitus (IDDM) or juvenile-onset diabetes, may account for 5 percent to 10 percent of all diagnosed cases of diabetes.
Risk factors are less well defined for Type 1 diabetes than for Type 2 diabetes, but autoimmune, genetic, and environmental factors are involved in the development of this type of diabetes.
Type 2:
Type 2 diabetes, was previously called non-insulin-dependent diabetes mellitus (NIDDM) or adult-onset diabetes. Type 2 diabetes may account for about 90 percent to 95 percent of all diagnosed cases of diabetes.
What causes type 1 diabetes?
Type 1 diabetes is caused by a lack of insulin due to the destruction of insulin-producing beta cells in the pancreas.
In type 1 diabetes—an autoimmune disease—the body’s immune system attacks and destroys the beta cells.
Normally, the immune system protects the body from infection by identifying and destroying bacteria, viruses, and other potentially harmful foreign substances.
But in autoimmune diseases, the immune system attacks the body’s own cells. In type 1 diabetes, beta cell destruction may take place over several years, but symptoms of the disease usually develop over a short period of time.
Type 1 diabetes typically occurs in children and young adults, though it can appear at any age. In the past, type 1 diabetes was called juvenile diabetes or insulin-dependent diabetes mellitus.
Genetic Susceptibility
Heredity plays an important part in determining who is likely to develop type 1 diabetes. Genes are passed down from biological parent to child.
Genes carry instructions for making proteins that are needed for the body’s cells to function. Many genes, as well as interactions among genes, are thought to influence susceptibility to and protection from type 1 diabetes.
The key genes may vary in different population groups. Variations in genes that affect more than 1 percent of a population group are called gene variants.
Certain gene variants that carry instructions for making proteins called human leukocyte antigens (HLAs) on white blood cells are linked to the risk of developing type 1 diabetes.
The proteins produced by HLA genes help determine whether the immune system recognizes a cell as part of the body or as foreign material.
Some combinations of HLA gene variants predict that a person will be at higher risk for type 1 diabetes, while other combinations are protective or have no effect on risk.
While HLA genes are the major risk genes for type 1 diabetes, many additional risk genes or gene regions have been found.
Not only can these genes help identify people at risk for type 1 diabetes, but they also provide important clues to help scientists better understand how the disease develops and identify potential targets for therapy and prevention.
Genetic testing can show what types of HLA genes a person carries and can reveal other genes linked to diabetes.
However, most genetic testing is done in a research setting and is not yet available to individuals.
Scientists are studying how the results of genetic testing can be used to improve type 1 diabetes prevention or treatment.
Autoimmune Destruction of Beta Cells
In type 1 diabetes, white blood cells called T cells attack and destroy beta cells. The process begins well before diabetes symptoms appear and continues after diagnosis.
Often, type 1 diabetes is not diagnosed until most beta cells have already been destroyed. At this point, a person needs daily insulin treatment to survive.
Finding ways to modify or stop this autoimmune process and preserve beta cell function is a major focus of current scientific research.
Recent research suggests insulin itself may be a key trigger of the immune attack on beta cells. The immune systems of people who are susceptible to developing type 1 diabetes respond to insulin as if it were a foreign substance, or antigen.
To combat antigens, the body makes proteins called antibodies. Antibodies to insulin and other proteins produced by beta cells are found in people with type 1 diabetes. Researchers test for these antibodies to help identify people at increased risk of developing the disease.
Testing the types and levels of antibodies in the blood can help determine whether a person has type 1 diabetes, LADA, or another type of diabetes.
Environmental Factors
Environmental factors, such as foods, viruses, and toxins, may play a role in the development of type 1 diabetes, but the exact nature of their role has not been determined.
Some theories suggest that environmental factors trigger the autoimmune destruction of beta cells in people with a genetic susceptibility to diabetes.
Other theories suggest that environmental factors play an ongoing role in diabetes, even after diagnosis.
Viruses and infections. A virus cannot cause diabetes on its own, but people are sometimes diagnosed with type 1 diabetes during or after a viral infection, suggesting a link between the two.
Also, the onset of type 1 diabetes occurs more frequently during the winter when viral infections are more common. Viruses possibly associated with type 1 diabetes include coxsackievirus B, cytomegalovirus, adenovirus, rubella, and mumps.
Scientists have described several ways these viruses may damage or destroy beta cells or possibly trigger an autoimmune response in susceptible people.
For example:
Anti-islet antibodies have been found in patients with congenital rubella syndrome, and cytomegalovirus has been associated with significant beta cell damage and acute pancreatitis–inflammation of the pancreas.
Scientists are trying to identify a virus that can cause type 1 diabetes so that a vaccine might be developed to prevent the disease.
Infant feeding practices. Some studies have suggested that dietary factors may raise or lower the risk of developing type 1 diabetes.
For example:
Breastfed infants and infants receiving vitamin D supplements may have a reduced risk of developing type 1 diabetes, while early exposure to cow’s milk and cereal proteins may increase risk. More research is needed to clarify how infant nutrition affects the risk for type 1 diabetes.
Risk factors for Type 2 diabetes:
Include older age, obesity, and family history of diabetes, prior history of gestational diabetes, impaired glucose tolerance, physical inactivity, and race/ethnicity.
African Americans, Hispanic/Latino Americans, American Indians, and some Asian Americans and Pacific Islanders are at particularly high risk for type 2 diabetes.
What is gestational diabetes?
Gestational diabetes is a type of diabetes that develops only during pregnancy. Diabetes means your blood glucose, also called blood sugar, is too high. Your body uses glucose for energy. Too much glucose in your blood is not good for you or your baby.
Gestational diabetes is usually diagnosed during late pregnancy. If you are diagnosed with diabetes earlier in your pregnancy, you may have had diabetes before you became pregnant.
Treating gestational diabetes can help both you and your baby stay healthy. You can protect your baby and yourself by taking action right away to control your blood glucose levels.
Gestational diabetes develops in 2 percent to 5 percent of all pregnancies but usually disappears when a pregnancy is over.
Gestational diabetes occurs more frequently in African Americans, Hispanic/Latino Americans, American Indians, and people with a family history of diabetes than in other groups.
Obesity is also associated with higher risk. Women who have had gestational diabetes are at increased risk for later developing Type 2 diabetes.
In some studies, nearly 40 percent of women with a history of gestational diabetes developed diabetes in the future 2- 3.
Other specific types of diabetes result from specific genetic syndromes, surgery, drugs, malnutrition, infections, and other illnesses.
Such types of diabetes may account for 1 percent to 2 percent of all diagnosed cases of diabetes.
What causes gestational diabetes?
Gestational diabetes happens when your body can't make enough insulin during pregnancy. Insulin is a hormone made in your pancreas, an organ located behind your stomach. Insulin helps your body use glucose for energy and helps control your blood glucose levels.
During pregnancy, your body makes more hormones and goes through other changes, such as weight gain. These changes cause your body's cells to use insulin less effectively, a condition called insulin resistance.
Insulin resistance increases your body's need for insulin. If your pancreas can't make enough insulin, you will have gestational diabetes.
All pregnant women have some insulin resistance during late pregnancy. However, some women have insulin resistance even before they get pregnant, usually because they are overweight.
These women start pregnancy with an increased need for insulin and are more likely to have gestational diabetes.
FAQS:
What are my chances of getting gestational diabetes?
Your chances of getting gestational diabetes are higher if you
-
are overweight
-
have had gestational diabetes before
-
have given birth to a baby weighing more than 9 pounds
-
have a parent, brother, or sister with type 2 diabetes
-
have prediabetes, meaning your blood glucose levels are higher than normal yet not high enough for a diagnosis of diabetes
-
are African American, American Indian, Asian American, Hispanic/Latina, or Pacific Islander American
-
have a hormonal disorder called polycystic ovary syndrome, also known as PCOS
How can I lower my chances of getting gestational diabetes?
If you are thinking about getting pregnant and are overweight, you can lower your chances of getting gestational diabetes by
-
losing extra weight.
-
increasing your physical activity level before you get pregnant.
Taking these steps can improve how your body uses insulin and help your blood glucose levels stay normal.
Once you are pregnant, you should not try to lose weight. You need to gain some weight for your baby to be healthy. However, gaining too much weight too quickly may increase your chances of getting gestational diabetes.
Your doctor will tell you how much weight gain and physical activity during pregnancy are right for you.
When will I be tested for gestational diabetes?
You will probably be tested for gestational diabetes between weeks 24 and 28 of your pregnancy.
If you have a higher chance of getting gestational diabetes, your doctor may test for diabetes during the first visit after you become pregnant.
If your blood glucose level is above normal at that time, you may be diagnosed with diabetes rather than gestational diabetes.
How is gestational diabetes diagnosed?
Doctors use blood tests to diagnose gestational diabetes. All diabetes blood tests involve drawing blood at a doctor's office or a commercial facility. Blood samples are sent to a lab for analysis.
Treatment for Type 2 diabetes Treatment typically includes:
-
Diet control exercise.
-
Home blood glucose testing.
-
And in some cases, oral medication and/or insulin. Approximately 40 percent of people with type 2 diabetes require insulin injections.
Screening Glucose Challenge Test
For this test, you will drink a sugary beverage and have your blood glucose level checked an hour later. This test can be done at any time of the day. If the results are above normal, you may need to have an oral glucose tolerance test.
Oral Glucose Tolerance Test
You will need to fast for at least 8 hours before the test. Fasting means having nothing to eat or drink except water. Your doctor will give you other instructions to follow before the test.
Your fasting blood glucose level will be checked before the test begins. Then you will drink a sugary beverage. Your blood glucose levels will be checked 1 hour, 2 hours, and possibly 3 hours later. Your doctor will use your test results to find out whether you have gestational diabetes.
How will gestational diabetes affect my baby?
If you have high blood glucose levels because your gestational diabetes is not under control, your baby will also have high blood glucose.
Your baby's pancreas will have to make extra insulin to control the high blood glucose. The extra glucose in your baby's blood is stored as fat.
Untreated or uncontrolled gestational diabetes can cause problems for your baby, such as
-
Being born with a larger than normal body—a condition called macrosomia—which can make delivery difficult and more dangerous for your baby.
-
having low blood glucose, also called hypoglycemia, right after birth
-
having breathing problems, a condition called respiratory distress syndrome
-
having a higher chance of dying before or soon after birth
Your baby also might be born with jaundice. Jaundice is more common in newborns of mothers who had diabetes during their pregnancy. With jaundice, the skin and whites of the eyes turn yellow.
Jaundice usually goes away, but your baby may need to be placed under special lights to help. Making sure your baby gets plenty of milk from breastfeeding will also help the jaundice go away.
Your baby will be more likely to become overweight and develop type 2 diabetes as he or she grows up.
Will I need extra tests during pregnancy to check my baby's health?
If you have gestational diabetes, your doctor may recommend that you have some extra tests to check your baby's health, such as:
-
Ultrasound exams, which use sound waves to make images that show your baby's growth and whether your baby is larger than normal.
-
A nonstress test, which uses a monitor placed on your abdomen to check whether your baby's heart rate increases as it should when your baby is active.
-
Kick counts to check the time between your baby's movements.
How will gestational diabetes affect me?
Gestational diabetes may increase your chances of:
-
Having high blood pressure and too much protein in the urine, a condition called preeclampsia.
-
Having surgery—called a cesarean section or c-section—to deliver your baby because your baby may be large.
-
Becoming depressed.
-
Developing type 2 diabetes and the problems that can come with this disease.
Preeclampsia:
Preeclampsia occurs during the second half of pregnancy. If not treated, preeclampsia can cause problems for you and your baby that could cause death.
The only cure for preeclampsia is to give birth. If you develop preeclampsia late in your pregnancy, you may need to have a cesarean section to deliver your baby early.
If you develop preeclampsia earlier, you may need bed rest and medicines, or you may have to be hospitalized to allow your baby to develop as much as possible before delivery.
Depression:
Depression can make you too tired to manage your diabetes and care for your baby. If during or after your pregnancy you feel anxious, sad, or unable to cope with the changes you are facing, talk with your health care team. Depression can be treated.
Your health care team may suggest ways you can get support and help to feel better. Remember, in order to take care of your baby, you must first take care of yourself.
Checkups:
Keep up with your checkups. “Feeling fine” does not mean you should skip any appointments. Women with gestational diabetes often have no symptoms. Your health care team will be on the lookout for any problems from gestational diabetes.
After Giving Birth:
Your diabetes will probably go away after your baby is born. However, even if your diabetes goes away after the birth, you:
-
May have gestational diabetes if you get pregnant again.
-
Will be more likely to have type 2 diabetes later in your life.
How is gestational diabetes treated?
Treating gestational diabetes means taking steps to keep your blood glucose levels in a target range. Targets are numbers you aim for. Your doctor will help you set your targets. You will learn how to control your blood glucose using:
-
Healthy eating.
-
Physical activity.
-
Insulin shots, if needed.
Can diabetes be prevented?
A number of studies have shown that regular physical activity can significantly reduce the risk of developing type 2 diabetes. Type 2 diabetes is also associated with obesity.
Is there a cure for diabetes?
In response to the growing health burden of diabetes mellitus (diabetes), the diabetes community has three choices:
-
Prevent diabetes.
-
Cure diabetes.
-
And take better care of people with diabetes to prevent devastating complications. All three approaches are actively being pursued by the US Department of Health and Human Services.
Some of what causes diabetes type 2
Insulin Resistance
Insulin resistance is a common condition in people who are overweight or obese, have excess abdominal fat, and are not physically active. Muscle, fat, and liver cells stop responding properly to insulin, forcing the pancreas to compensate by producing extra insulin.
As long as beta cells are able to produce enough insulin, blood glucose levels stay in the normal range. But when insulin production falters because of beta cell dysfunction, glucose levels rise, leading to prediabetes or diabetes.
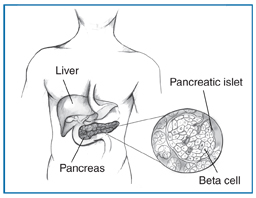
Abnormal Glucose Production by the Liver
In some people with diabetes, an abnormal increase in glucose production by the liver also contributes to high blood glucose levels. Normally, the pancreas releases the hormone glucagon when blood glucose and insulin levels are low.
Glucagon stimulates the liver to produce glucose and release it into the bloodstream. But when blood glucose and insulin levels are high after a meal, glucagon levels drop, and the liver stores excess glucose for later, when it is needed.
For reasons not completely understood, in many people with diabetes, glucagon levels stay higher than needed. High glucagon levels cause the liver to produce unneeded glucose, which contributes to high blood glucose levels. Metformin, the most commonly used drug to treat type 2 diabetes, reduces glucose production by the liver.
The Roles of Insulin and Glucagon in Normal Blood Glucose Regulation
A healthy person’s body keeps blood glucose levels in a normal range through several complex mechanisms. Insulin and glucagon, two hormones made in the pancreas, help regulate blood glucose levels:
-
Insulin, made by beta cells, lowers elevated blood glucose levels.
-
Glucagon, made by alpha cells, raises low blood glucose levels. When blood glucose levels rise after a meal, the pancreas releases insulin into the blood.
-
Insulin helps muscle, fat, and liver cells absorb glucose from the bloodstream, lowering blood glucose levels.
-
Insulin stimulates the liver and muscle tissue to store excess glucose. The stored form of glucose is called glycogen.
-
Insulin also lowers blood glucose levels by reducing glucose production in the liver.
-
When blood glucose levels drop overnight or due to a skipped meal or heavy exercise, the pancreas releases glucagon into the blood.
-
Glucagon signals the liver and muscle tissue to break down glycogen into glucose, which enters the bloodstream and raises blood glucose levels.
-
If the body needs more glucose, glucagon stimulates the liver to make glucose from amino acids.
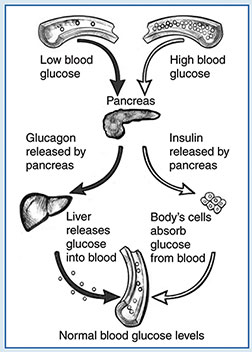
Insulin and glucagon help regulate blood glucose levels.
Metabolic Syndrome
Metabolic syndrome, also called insulin resistance syndrome, refers to a group of conditions common in people with insulin resistance, including
-
higher than normal blood glucose levels
-
increased waist size due to excess abdominal fat
-
high blood pressure
-
abnormal levels of cholesterol and triglycerides in the blood
People with metabolic syndrome have an increased risk of developing type 2 diabetes and CVD.
Many studies have found that lifestyle changes, such as being physically active and losing excess weight, are the best ways to reverse metabolic syndrome, improve the body’s response to insulin, and reduce risk for type 2 diabetes and CVD.
Cell Signaling and Regulation
Cells communicate through a complex network of molecular signaling pathways. For example, on cell surfaces, insulin receptor molecules capture, or bind, insulin molecules circulating in the bloodstream.
This interaction between insulin and its receptor prompts the biochemical signals that enable the cells to absorb glucose from the blood and use it for energy.
Problems in cell signaling systems can set off a chain reaction that leads to diabetes or other diseases. Many studies have focused on how insulin signals cells to communicate and regulate action.
Beta Cell Dysfunction
Scientists think beta cell dysfunction is a key contributor to type 2 diabetes. Beta cell impairment can cause inadequate or abnormal patterns of insulin release. Also, beta cells may be damaged by high blood glucose itself, a condition called glucose toxicity.
Scientists have not determined the causes of beta cell dysfunction in most cases. Single gene defects lead to specific forms of diabetes called maturity-onset diabetes of the young (MODY). The genes involved regulate insulin production in the beta cells.
Although these forms of diabetes are rare, they provide clues as to how beta cell function may be affected by key regulatory factors. Other gene variants are involved in determining the number and function of beta cells.
But these variants account for only a small percentage of type 2 diabetes cases. Malnutrition early in life is also being investigated as a cause of beta cell dysfunction. The metabolic environment of the developing fetus may also create a predisposition for diabetes later in life.
Future Risk of Type 2 Diabetes
Because a woman’s hormones usually return to normal levels soon after giving birth, gestational diabetes disappears in most women after delivery.
However, women who have gestational diabetes are more likely to develop gestational diabetes with future pregnancies and develop type 2 diabetes.
Women with gestational diabetes should be tested for persistent diabetes 6 to 12 weeks after delivery and at least every 3 years thereafter.
Also, exposure to high glucose levels during gestation increases a child’s risk for becoming overweight or obese and for developing type 2 diabetes later on. The result may be a cycle of diabetes affecting multiple generations in a family.
For both mother and child, maintaining a healthy body weight and being physically active may help prevent type 2 diabetes.
Other Types and Causes of Diabetes
Other types of diabetes have a variety of possible causes.
Genetic Mutations Affecting Beta Cells, Insulin, and Insulin Action
Some relatively uncommon forms of diabetes known as monogenic diabetes are caused by mutations, or changes, in a single gene. These mutations are usually inherited, but sometimes the gene mutation occurs spontaneously.
Most of these gene mutations cause diabetes by reducing beta cells’ ability to produce insulin.
The most common types of monogenic diabetes are neonatal diabetes mellitus (NDM) and MODY. NDM occurs in the first 6 months of life. MODY is usually found during adolescence or early adulthood but sometimes is not diagnosed until later in life.
Other rare genetic mutations can cause diabetes by damaging the quality of insulin the body produces or by causing abnormalities in insulin receptors.
Other Genetic Diseases
Diabetes occurs in people with Down syndrome, Klinefelter syndrome, and Turner syndrome at higher rates than the general population.
Scientists are investigating whether genes that may predispose people to genetic syndromes also predispose th